Integrated discussion, ideas, links and more
Both Prenatal Yoga (Relax, Stretch and Breathe) and Mother and Baby Yoga include an integrated discussion or informal prenatal or parenting class. These discussions are always interested and varied after each session I share more information, ideas and links. Here are some of those follow ups, for anyone who might find them useful...
Informed Decision Making
The decisions that parents choose to make may be exactly what the doctor is recommending, but it is important that they have the opportunity to ask questions, find more information and decide for themselves, rather than simply being swept along by the hospital decision making or protocol. So in no way am I say you “should” challenge your healthcare professionals (not least because it is not my place to say that you “should” do anything - it is always your decision and your choice). But I am saying that you have the right and that there is a great value in taking the time and having the confidence to ask questions, and if you wish to, to challenge the protocol or the discussion, or the healthcare professional. There is lots and lots more I could say about protocols and how and who they apply to, but it wont all fit here. However if you feel you are being pushed into decisions or courses of actions you or your partner don't feel comfortable with or don't feel right for you, please don't hesitate to get in touch - and of course try this EBRAIN tool.
A little bit about hypnobirthing
If you are interested in hypnobirthing I highly recommend having a look at https://www.kghypnobirthing.com. There are plenty of free resources, including tracks to download and listen to, and you will see wide variety of tracks (not all of them free) for many many different pregnancy and birth situations. There are also some really lovely daily affirmations, sent to your inbox, if you like affirmations. There are lots of different hypnobirthing resources available. I particularly like KGhypnobirthing, that is who I chose to do my hypnobirthing training with, but if you want suggestions of others please do say and I can recommend some others too).
I have done a little summary of three things from hypnobirthing that we talked about on Thursday - there is of course much more to it than these, but these might be really helpful.
One is about letting go of negative preconceptions about birth - and that can take time and practice, but little by little, as we learn more about birth and about ourselves and our babies, we can move to feel calm and positive about birth, even if that is not howe we felt about it when we first became pregnant. This is just as important for your birth supporters too! There are a myriad of ways of doing this - education, breathing and relaxation techniques, research and analysis, positive words….
Which leads us to a second point - protecting ourselves and our partners from hearing stories or experiences that disempower, or induce fear or unease. There are some helpful phrases that you or your partner might use as a shield - protecting yourselves from fear or stress, and also protecting your future birth experience (and sometimes you have to be really up front about this, even with birth professionals)
Thirdly, it takes practice and repetition - and that practice feels really good, helps you feel good right now, as well as supporting you for the birth you want (whatever those preferences are - hypnobirthing is helpful in every birth situation). It is never too late to start, and you don’t have to start a formal hypnobirthing course. Breathing, meditation, yoga, singing can all be your practice.
Taking care of your relationships after the baby is born
We covered a lot in our Partner’s Welcome session 16 May, and here are a few reminders and some link about what we talked about.
Our main topic was around relationships and some of the trigger points that are common for families with a new baby. The six most common topics of disagreement
are:
Sleep
For many/most families the important question is not “how do I get the baby to sleep more” but “how do we make sure that everyone in the family gets enough sleep”. Babies are quite good at making sure they get enough sleep, because they sleep during the day as well as at night. For the adults it can be more complicated, but often it is easier and more effective to adapt the adult schedule than try to make the baby sleep to a schedule. So some families will tag team, where one adult goes to bed early and gets up early and the other does the late shift. Or one adult does more night time parenting during the week and the other does more at the weekend. Maybe one adult will sleep with the baby (either in the same room or in the same bed) on some nights and the other on other nights. It is tiring, no matter what, but it can be less stressful for everyone to look at it like this, rather than focussing on the baby’s sleep schedule.
https://sarahockwell-smith.com/2015/04/15/how-long-should-babies-and-toddlers-sleep-for-infographic/. This infographic is great on a more realistic look at length of sleep and regularity of waking (spoiler alert, many babies carry on waking frequently through most or all of the first year).
There are some excellent resources here: https://www.basisonline.org.uk - this is the best evidence resource, with hundreds of clinical trials looking at safe and effective sleep. It also shares data and recommendations around co sleeping and how to do this safely. Around 70% of families in europe co sleep at some point in their child’s first year. For some that is their chosen way of sleeping (as it is in the majority of the population around the world), for many others it happens because the baby wont sleep in any other way, or because the parent falls asleep with the baby without meaning too.
Co sleeping can be done safely, as safely as a baby sleeping in their own crib so long as: 1. No one in the bed has been smoking in the past 24 hours. 2. No one in the bed has been taking drugs that make them sleep more heavily than normal. 3. No one in the bed is clinically obese. 4. You are sleeping on a firm, flat surface - so not a water bed or airbed and especially not a sofa or arm chair. Even if you don’t intend to ever co sleep, it is worth knowing how to do it safely, as a just in case - and to know that falling asleep in an arm chair or on a sofa with the baby is not safe (unless there is an awake adult int he room all the time as well), as this is when there can be a risk to the baby, if they slide between the adult and the side of the chair. If you feel tired much safe to sit or lie on the bed with the baby than in a chair.
Sleep consultants and sleep experts do exist, and there are all sorts of different styles. You do not have to sleep train (most people don’t), or follow the advice of a sleep expert, however if you are interested in learning more, Lyndsey Hookway is a very interesting, evidence based and empathetic person to follow. Here is her Instagram: https://www.instagram.com/lyndsey_hookway/?hl=en and there is some really good stuff on there, on all sorts of topics (including the question about siblings sharing a room that we talked about), so well worth having a browse through.
You might also like to have a listen to this episode of Child - which includes Helen Ball, who founded Basis, mentioned above, and also discusses sleep consultants and sleep training. https://www.bbc.co.uk/sounds/play/p0hhrq63
Perhaps the main message regarding sleep, is that every family does it their own way and that is absolutely fine. And as we said in class, often people are not entirely honest about their baby’s sleep, so please dont compare too much.
Pain management
We covered a lot in our Thursday evening RSB session about pain management techniques, from
pharmacological pain management to the significance of psychological confidence in yourself and your body with a little detour via some of the amazing anatomical changes in a woman’s body that
happens when she gives birth.
Here is a quick reminder of the typical ladder of support for those intense sensations that is used in
Basel:
The foundation of all labour and birth paî management is staying as relaxed as possible. Breathe, dim
lighting, massage, music, movement, warm baths, laughing, yoga stretches, encouragement, smooching, fresh air, distractions may help, each person will have their own particular combination, so it
can be helpful to think of what you do now when you are tired, or anxious or have back ache (or what you used to do when you had period pains). Having support and encouragement from
someone you trust has been shown to help enormously too.
These are all things you can do at home, in early labour, it continue doing them too as the
labour progresses and you move to the hospital or the geburtshaus.
Once you are in hospital or geburtshaus you are very likely to be offered homeopathy, aromatherapy or
acupuncture as an additional aid. Once you are in active labour (contractions lasting a minute and coming every five minutes or more frequently, or, three or more contractions within ten minutes)
you might choose to go in the birthing pool.
There is lots of evidence on the effectiveness and safety of birthing pools. They have been shown to
be an excellent form of pain relief, time in the birthing pool helps reduce the risk of perineal tearing, and makes a straightforward birth significantly more likely. You can choose to go in the
pool or not, choose to stay in for just a short time, get in and out and back in again, or to stay in and birth the baby in the water.
Also now available in a few places (Liestalspital and the midwife led unit at the Unispital is gas and
air (laughing gas/nitrous oxide). It is present in other departments in other hospitals so as we discussed you could ask for it elsewhere (or get your partner to go and ask for it on your
behalf).
The healthcare team may also suggest using pethidine which is an opiate based injection. It is not
widely used but is sometimes offered, particularly in the earlier stages of an induction.
Finally, and very widely used is epidural/PDA. Once you have an epidural in place you can’t go into
the birth pool, but with the low dose epidurals currently used the woman does still have a range of movement and positions available to her, tho she needs to stay on or close to the
bed.
Caesarean Birth
This is the Caesarean Birth Padlet that I share as part of the Preparing for Parenthood classes I offer. There is masses of information in it - links to films, articles, information PDFs, research articles and so on. If you have time to have a quick look at it this weekend so you know what is there, I would recommend it, so you can then come back to it as and when it feels appropriate. https://padlet.com/susieroseatkinson/caesarean-birth-fm6r7jqsl2fmtygn
TL:DR summary would be:
Caesarean birth is major surgery so recovery takes time and families need lots of support and help in the first month.
Caesarean birth may delay breastmilk arrival - breastfeeding in the first 12 weeks is hard work for everyone, and everyone needs support and reassurance, this might be particulary true after a caesarean birth, and it can be really helpful to have a rdv with an IBCLC before a planned caearean, and of course after any birth it can be a really helpful thing to do.
The phrase “emergency caesarean” makes it sound as though it will be drama, rush, blue flashing lights. In reality an emergency caesarean is any caesarean that happens when a woman is already in labour, and is preceded by rounds of monitoring, tests and discussions - there is plenty of time to ask questions and ensure that the family understand what is happening and why, so they can make an informed decision (and this is really important for protecting the families postnatal mental health). Very occasionally a “crash caesarean” is required, where the operation does have to be done fast (within ten minutes) but this is very unusual.
Strengthening and relaxing the pelvic floor: better than a tight pelvic floor
Recently in Prenatal Relax, Stretch and Breathe we talked a lot about the pelvic floor, and
how to strengthen, and how to relax it, going on to doing lots of yoga positions to hep with both of these. A strong pelvic floor is important to help with stress incontinence during and
after pregnancy. Did you know by the end of pregnancy the pelvic floor will be directly supporting, on average 3,5kg of baby, 1kg amniotic fluid (about a litre), 700g placenta? No wonder it
needs support. However during birth the pelvic floor needs to relax to be able to open to allow the baby to pass through it as it descends through the vagina. A tight pelvic floor
makes that passage more difficult.
Kegel exercises are often the first line of pelvic floor care during pregnancy, yet evidence shows that keel exercise may lead to a tight pelvic floor, but not necessarily a strong
pelvic floor, and one that may not open easily. This interview with Katy Bowman explains more. Katy Bowman is a biomechanists and a pelvic floor expert and she advocates squats
and other movements to strengthen the pelvic floor rather than tighten it. They are many of the same movements that the postnatal midwives use helping new mothers re find their pelvic
floors (within days after the birth). A BIG CAVEAT: if your doctor has advise against doing deep squats (for example because of a short cervix) or if your baby is more than 33 weeks
gestation and is in a breech position, do not do deep squats. https://bestdoulas.com/wp-content/uploads/2020/07/squats-not-kegels.pdf
For those of you who use FB, this is an excellent post from Deborah Neiger, an independent midwife about the importance of having a relaxed pelvic floor during birth, and techniques to help you achieve this. https://www.facebook.com/story.php?story_fbid=pfbid02FoUbxcyosueGFLnuS8BgxSXwXkv7WLiUcbaFwk9E37S5FvzXQGKR7mC3TUFPxcDBl&id=100000317994095&paipv=0&eav=AfYZwlCa7xB0VZOen12VezPCmJAbcxzgUf44Llx4Bpz675uUpz78mfkumTvcGHzGaNA&_rdr
Positions for a straightforward birth
In our Partners Welcome session in October we discussed how the baby positions itself in the pelvis in the last trimester and how different positions and movements can help the baby get into an
ideal position for birth. The simplest rout through the pelvis for the baby is when they are had down, and looking diagonally backwards towards the mother's right kidney. This means
that the baby's head fits neatly into the shape of the pelvis at the top. The baby rotates int he pelvis so that the shoulders it in at the top, and the baby's head fits neatly through the
pelvic outlet. They then rotate again so that the shoulders can easily pass through pelvic outlet.
The baby is floating in amniotic fluid, so the position the mother is in during late pregnancy and during labour affects how the baby is positioned in the uterus. Positions that are forward
leaning, rather than lying back, help the baby rotate into that ideal backward facing position. Maternal positions that open up the pelvic outlet, such as those that are forward leaning
help make more space for the baby to go through the pelvis. Because the pelvis is flexible, when the mother rocks and sways or circle her hips she creates more space in the pelvis
for the baby as it travels through.
Try positions such as:
Hugging your partner and swaying with them
Leaning forward over the table or the sofa back
Sitting backwards, leaning over the back of a chair
Kneeling on all fours, leaning on a birth ball, chair seat or your partner
Lying on your side
It can be so helpful for some couples for the partner to physically support the woman in labour, encouraging her to lean on them. This not only provides physical support and allows the woman to rest, it also helps lift her oxytocin levels (and those of her partners) to help keep the birth moving forward. Partners can also be active in rocking and swaying, giving women the benefit of movement, without having to use the energy to do it all themselves.
For more information about positions for birth and optimal foetal positioning, have a look at https://www.spinningbabies.com/ and see the images below.


Thermoregulation between babies and their carers
On a very hot evening in August our discussion time in Prenatal Relax, Stretch and Breathe included how might one keep your baby cool during hot weather and warm during warm weather.
Babies rely on their adult carers to help them thermoregulate and carrying a baby is a great way to do this. Carrying a baby in a sling or a baby carriers helps the adult monitor the baby's
temperature constantly and helps cool them down through adult sweating and or warm them up from the adult's body temperature, or to change the environment around them - finding shade, or
warmth depending on what the baby needs.
Caring for a baby in extremes of weather is hard. The ideal temperature for a baby's sleeping place is 16-18 degrees (according to the Lullaby Trust Safe sleep Guidelines - as a side note it shows that guidelines are only guidelines and not rules - since sometimes guidelines simply can't be met), but the Lullaby Trust has excellent suggestions for caring for your baby during hot temperatures: https://www.lullabytrust.org.uk/safer-sleep-advice/baby-summer-safety/ and https://www.lullabytrust.org.uk/safer-sleep-advice/baby-room-temperature/. In cold weather it can be tempting to heap lots of warm and cuddly things in the baby's sleeping space to keep them warm, but again, the Lullaby Trust has excellent guidance on keeping your baby warm without the risk of them overheating: https://www.lullabytrust.org.uk/safer-sleep-advice/safer-sleep-winter/
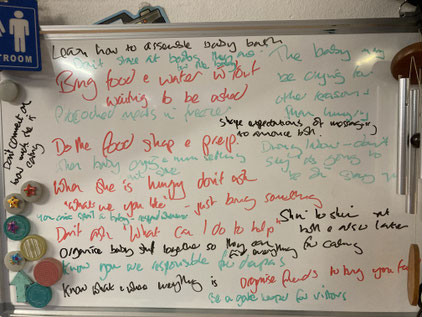
Suggestions for support for new mothers, from new mothers
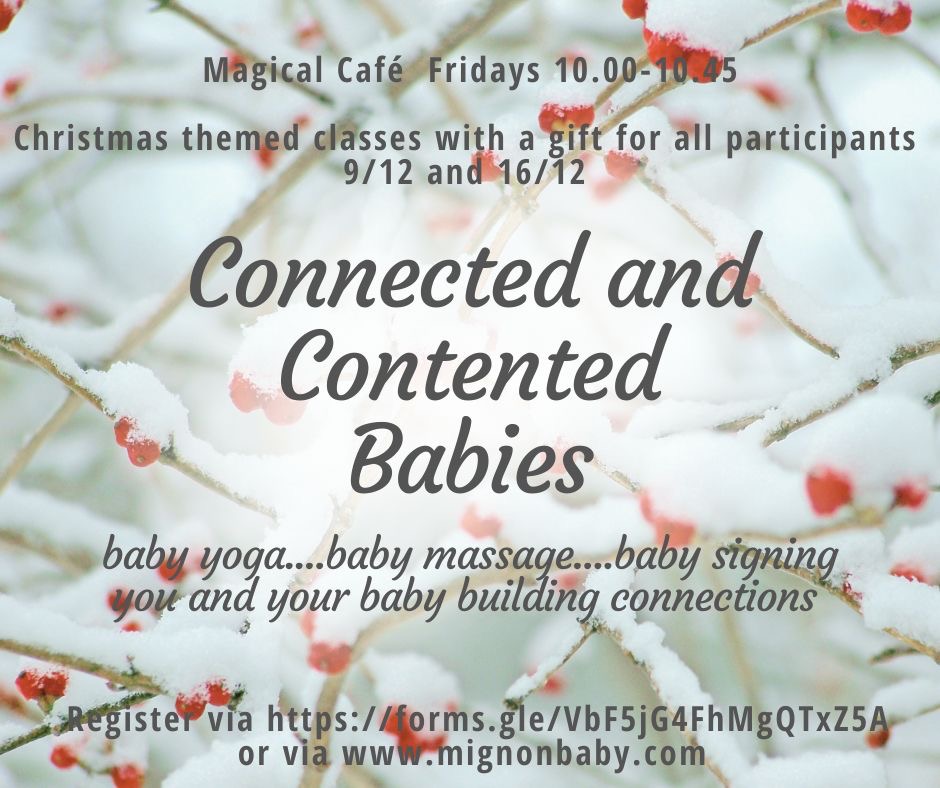
Each week I run a Connected and Contented Baby Sessions, incorporating Baby Yoga, Baby Massage and Baby Signing, and focusing on connections – within the baby’s body and brain, between the baby and their caregiver, and in the community.
I asked this group to help me with some suggestions for ways the not-birthing parent can support the parent who birthed during the early postpartum period., particularly around feeding but also generally. They did not disappoint! A wealth of suggestions, some very personal and individual (and some which made us ask “what’s the back story?!?”) and many that were shared across the whole group. Of course not all of these suggestions are right for every family situation, but I share them with you here to learn from, or at least use as an insight into some of the priorities and pressure points for a new family. I hope it will be helpful.
A huge thank you to the group for their time and ideas, I hope I have summarized them appropriately and accurately. In this case the group happened all to be women, but either or both parents are always welcome at the Connected and Contented baby sessions.
Suggestions: these may or may not apply in your situation and relationship!
Bring food and drink to her without waiting to be asked
Have plenty of meals ready to eat in the freezer. They don’t have to be homecooked!
Do all the food shopping and prepping.
When she is hungry, don’t ask her what she wants to eat and drink. Use your initiative and bring her something you know she likes.
Organise friends to bring you meals.
Don’t comment on how much she is eating!
Learn how to assemble the baby bath.
Know what all the different baby equipment and clothes are, what your partner calls them and where they are kept so you can find them easily.
Do all the unpacking and building of baby equipment together.
Know that you are responsible for diapers.
Know that you can’t spoil a new born baby, and protect your new family from people offering unhelpful advice that suggests otherwise.
Don’t forget that skin to skin is wonderful at birth but also is fantastic later for calming the baby.
During labour don’t talk too much (and don’t say “it’s all going to be fine”).
Don’t look at the woman’s breasts, even if they are bigger than ever before, it may make her uncomfortable, and she may feel they are for the baby not for you.
The baby may be crying for some reason other than hunger, and so it doesn’t always have to be the mother that comforts/feeds the baby when they cry.
Don’t stare at her whilst she is settling a crying baby.
Shape family expectations about hearing and sharing news of the baby’s arrival, so people are not upset if they do not hear news straight away.
Be a gate keeper for visitors.
I hope these suggestions, which come from the hearts of seven wonderful women with babies between 4 and 9 months may be helpful. I hope they might prompt discussion and help you make your postnatal plan as a family.
Pre and Postnatal Mental Health
Pre and Postnatal mental health issues are becoming more widely talked about, but are still probably under- discussed, and under-diagnosed.
Our RSB session on 22 June focused particularly on postnatal mental health and some of the most common situations. Here are three scenarios, as a new parent might describe their situation to a sympathetic listener....and some thoughts about them:
1:
Henry is three days old , and my partner Paula is not coping well and I don't know how to help. Paula cries at everything (much more than Henry), even adverts on the TV can make her cry. breastfeeding is harder than we expected but when I suggested making a bottle of formula for Henry, Paula shouted at me and refused. Henry hates his cot and needs to be held all the time so we are taking it in turns and we are both exhausted. The apartment is a mess and we are living on takeaways and cereal. Is this normal?
Yes - this does all sound really normal. A really normal response to having a baby, and also a normal case of BABY BLUES. Baby Blues occurs in about 70% of women between 3-5 days after the birth of their baby. It is a hormonal and emotional rollercoaster, as the pregnancy hormones drop and the breastfeeding and nurturing hormones rise (and still happens in women who are not breastfeeding). It usually last three or four days, and then passes. It needs empathy, support, encouragement and reassurance, but not medical treatment.
2:
Our gorgeous baby Stan was born just two months ago. My partner Fred took the parental leave at the time and we enjoyed learning how to be parents together. We laughed a lot at our incompetence and what a state we looked by the end of the day. It was crazy but we made the best of it.
But things have changed and he’s just not himself now. I know we are tired, but I think this is something more, something worrying. He’s finding it hard to concentrate at work and so he’s worried he might be letting people down there. He keeps making us lists to make sure we don’t forget anything important but then gets stressed if we can’t get it all done. He’s great with baby Stan but I don’t think he believes me when I tell him that. He’s just not enjoying being a Dad as much as we thought he would. Is this normal?
Yes, this is very normal. Having a baby does change us and most parents feel overwhelmed at times, and often a lot of the time. However Fred's partner is right to be worried about them. There are signs of POSTNATAL DEPRESSION in this description. Anxiety and stress, inability to concentrate, feeling that one is a bad parent are all common features in postnatal depression. Fathers are vulnerable to postnatal depression just as mothers are (and sadly, if one partner has postnatal depression that puts the other partner at a higher risk).
3. I’m so worried about my partner Juliana. Our beautiful, longed for baby Archie was born 12 weeks ago and is getting more and more gorgeous by the day. But Juliana is not doing so well. She seems to have lost her sparkle -we are tired I know but it’s more than that. She’s not talking to her friends as much. She puts on a brave act for the BCT group, but it wears her out and she thinks they are all doing better than her.
I’m doing my best to support her. I’ve taken extra leave from work so I can take care of Archie and let her sleep.
We should be enjoying this more. I imagined us snuggled up on the sofa watching Netflix and cuddling Archie. She says she’s too tired for TV even, that she can’t follow the story. It’s hard to get her to come for a walk even. I think she would forget to eat if I didn’t keep putting food in front of her.
She keeps saying she thinks she’s a terrible mum but when I look at how she is with Archie I am so proud of her and he clearly adores her. Is this normal?
As with scenario 2, many things in this story are normal for all new parents - tiredness, feelings of uncertainty or imposter syndrome, difficulty in focussing, feeling overwhelmed. These are all really common feelings in the first four or six weeks with a new baby, this is partly why PND is rarely diagnosed before 1 month. For most families, the feelings over confusion, overwhelm, and uncertainty start to diminish after about six week, the parents realise that whilst they are still learning all the time, facing new experiences with their babies, still tired and worried about whether they are doing things right, they have gained confidence and recognise that they are doing okay. Some parents don't, and that is what seems to be being described here, and that is where you might look for some help and support for PND.
Here is a fourth scenario:
I’m having a really hard time and I need to get some help from somewhere. Our baby Ralph is five weeks old now, but my partner Suze still hasn’t really got it together.
I’m back at work in the home office, but I’m constantly interrupted by the sound of Ralph crying. When I come downstairs for lunch the place looks like a bomb site and there is never any food made so I end up just making a sandwich and eating it upstairs in the office.
I have to cook every evening and then I get a load of abuse for not clearing up properly.
I think Suze looks amazing, but she says she feels like her body isn’t hers anymore. I tried to give her a cuddle, but she pushed me away said “sex is definitely out of the question for the foreseeable future” -it was just a cuddle. I’m finding that tough to be honest. We used to be so close.
I’m starting to suspect she has postnatal depression and want to call a doctor....
Is this postnatal depression? I would propose that Suze, the mother, does not have PND at this point. However, the partner writing is perhaps vulnerable to PND. He/she seems to be struggling with the changes that come with having a new baby. Whilst they come across, in this scenario as being a bit of an idiot, in fact they deserve sympathy and support to manage this transition and their feelings about it, in order to protect themselves and their partners against postnatal depression.
Risk factors and triggers for PND:
There are various factors that have been shown to increase the risk of PND, being aware of these may be helpful. The idea is not to make people worry but to help them take preventative or early action.
- Family or personal history of depression (including a parent who suffered from PND)
- Stressful life events (such as a bereavement, a relocation, a separation, a house move, a career change or end)
- Traumatic birth, birth disappointment or feeling disempowered during birth (that is, things happened during the birth that you weren't consulted on or you felt pressured into making decisions without enough time or information to make an informed decision)
- Pregnancy complications
- Fertility issue or previous pregnancy loss
- Relationship difficulties
- Family violence and controlling behaviours
- History of abuse or trauma
- Financial difficulties
- Difficult child hood experiences
- Limited social support
Further reading and useful resources:
https://www.nhs.uk/conditions/baby/support-and-services/feeling-depressed-after-childbirth/
https://www.rcpsych.ac.uk/mental-health/problems-disorders/post-natal-depression
Local resources and support:
https://baselchildrenstrust.ch/
https://postpartale-depression.ch/fr/
Please do not hesitate to get in touch if you are worried about yourself, your partner or a friend and need help in finding support for them.
Most common treatment for PND in Basel is a combination of counselling, support at home, and often drug therapy. Medical help can be accessed via your midwife, your paediatrician, your hausartz, your gynae, directly from the unispital frauenklinik. Please do not hesitate to ask for help.
Prenatal yoga stretches to help with sciatica
Prenatal Yoga for Sciatica
Sciatica is caused by compression of the sciatic nerve and is felt as pains down the inside of the leg, or numbness or tingling.
Good posture and keeping mobile rather than static (try using an exercise ball instead of a chair if you have to sit for long periods) can help, as can heat packs or hot water bottles.
There are a number of yoga stretches that can be safely down during pregnancy that can help. However, as you do these stretches, listen to your body and stop or adapt them if they feel uncomfortable.
Downward facing dog – in late pregnancy hold for no more than 30 seconds. Avoid this pose if you have high blood pressure or carpal tunnel syndrome.
Seated or reclining pigeon pose – either or a chair, or lying down, one ankle resting on the opposite knee.
Supported forward bend – use a chair or the wall for this half way forward fold. This gives a big calf and ham string stretch as well as releasing pressure on the back and the pelvis. Use the wall or the chair to help you up as you come out of the pose.
Forward lunge – this can be a static lunge, or even better with a gentle rock backwards and forwards. Ensure that the knee is not extending beyond the ankle.
For a half hour prenatal yoga sequence for sciatica I like this film:
https://www.youtube.com/watch?v=SFMoku8trIA
Massage in pregnancy and labour
In RSB on 11 November, we practiced some massage techniques for pregnancy and for labour. Massage has been shown to be effective at reducing sensations of pain during pregnancy and labour without negative side effects (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2870995/). In general, most women find that smooth strokes with the palms of the hands (or a massage toy) on the back, the lower back, the thighs, shoulders and down the arms can be really helpful. A firmer or stronger pressure, particularly on the sacrum or the lower back can be especially helpful as a counter pressure to the contractions. Experiment with the level of pressure and make sure that you keep communicating between you the two of you as to what feels good and what doesn't.
Practice during pregnancy as been shown to increase the benefits of massage during labour, so do keep practicing during pregnancy. It is really important that the person doing the massage is as comfortable (and relaxed) as the person getting the massage, so take your time to get comfortable (both of you), to take some deep breaths and keep the massage strokes really slow. Breathing (slowly) in time with the massage strokes can increase the relaxing effect of both the deep breathing and the massage.
This link has a good explanation about the benefits of massage and some different techniques to try.
https://evidencebasedbirth.com/massage-for-pain-relief-during-labor/
Hypno birth resources
In RSB on Tuesday 26 May we were discussing how hypnosis birth style tracks can be useful at many different stages of pregnancy as well as during birth. Here are link to more information about some off the different hypno birth offerings from different organisations, including free tracks to download.
These are not specific recommendations, I suggested that you browse through them all and listen to some of the sample tracks to ensure that you like the sound of the practitioners voice. There will also be other resources available in different languages, google is great for this.
http://www.hypnobirthingplace.co.uk/pregnancy-birth-free-support - tracks, affirmations and activities, plus details about classes
https://thewisehippo.com/shop/ - free tracks to download, including some for morning sickness, plus details about classes
https://www.kghypnobirthing.com/ - classes, resources and free downloads
https://www.natalhypnotherapy.co.uk - the original UK offering (also available in a variety of languages), details about classes and packages plus downloads including for different stages of pregnancy and postnatal life
http://hypnobirthingus.wob-web.me - the original American hypnobirthing
For local classes (on line or in person when possible), there is the truly wonderful Menna Keyes:
https://www.facebook.com/mennakeyesdoula/
Perineal massage, a lot of good discussion and ideas:
There has been plenty of discussion this week on the RSB WhatsApp group about protecting the perineum during birth and how to avoid a tear on an episiotomy. Episiotomies are not done so frequently in Switzerland - ideally there won't be any damage to the perineum at all, and the midwives here are quite hands on to help with that, but a tear is considered preferable to a cut - as it will usually be less deep and heal more quickly and more strongly. An episiotomy is usually necessary for an assisted birth- one that uses ventouse or forceps.
Perineal massage, using water throughout the active labour (even if intermittently), spending time in the water or giving birth in the water, choosing particular positions and breathing patterns and making sure the midwife knows if you are fearful about tearing are probably all effective to prevent tearing. Interventions (eg induction, or augmentation) can cause a cascade of other interventions which may include (earlier) epidural and therefore reduced mobility, less optimal position for baby and so bigger stretch for the perineum, and more likely use of ventouse, and therefore episiotomy).
If it’s an option for you and appeals then the geburtshauses usually report extremely low rates of perineal trauma (for example 96% women have intact perineum at the Tagmond). This is partly because of the lower rate of interventions; the protocols about the length of time for stages of labour are different (more time, which again leads to fewer interventions like augmentation) and very high rates of water birth, plus women using a v wide range of positions to birth in. If a geburtshaus is not for you you can absolutely recreate those conditions in a hospital setting, you may need to be more of an advocate for yourself, to consider the effect of any interventions that are suggested (the ins and outs of why there are more interventions in hospitals than home births and birth houses are fascinating and complex).
So to help avoid stitches:
In advance:
- perineal massage from 34 weeks (if this feels okay for you - if it makes you feel really stressed then that might become counterproductive. There is research that shows that perineal massage from 34 weeks has a statistically significant effect on reducing tears - but equally there are many women who never do perineal massage and don't tear)
- pelvic balancing work and pelvic floor work, basically what we do in RSB
In labour:
- staying mobile, upright/forward leaning
- using the bath or birth pool
- choosing not to have an epidural, or keeping the epidural low dose
During the second stage/pushing stage/ as the baby’s head is emerging
- telling the midwife you are worried about tearing, she can be hands on and also suggest positions and breathing
- panting or doing steam train impressions when the baby’s head is crowning
- using all fours positions/Sphinx pose over squat positions (but the midwife will guide/coach you with this.)
I rather like this article on this topic
Some Yoga links and ideas:
Please stick within your limits and if anything feels uncomfortable please stop. Whether you are pregnant or have a small baby, now is not the time to be pushing yourself, instead yoga should be about finding what feels good and keeping yourself within that feel good place.
Some prenatal Yoga from Yoga with Adrienne (also nice with a small baby): https://youtu.be/0cKnStmV1dI
Some Spinning Babies Yoga moves from our regular RSB sessions. See also www.spinningbabies.com
Some Mindful Mama relaxations and affirmations to listen to: https://www.penguin.co.uk/articles/2016/mindful-hypnobirthing/
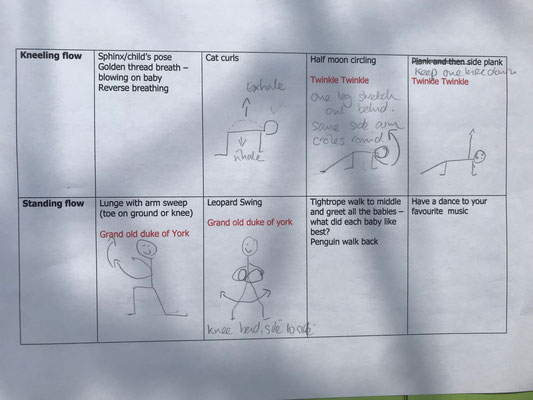
A Mother and Baby Yoga session, with sketch drawings and song ideas
Guidelines
RCOG guidelines on corona virus in pregnancy: https://www.rcog.org.uk/coronavirus-pregnancy
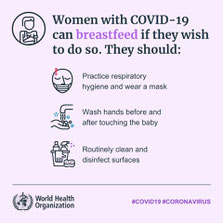
Coronavirus and Breastfeeding: https://www.llli.org/coronavirus/
Follow up from RSB discussions
Upcoming courses
Prenatal Relax, Stretch and Breathe

Gentle prenatal yoga, combined with discussion time, social support, breathing and relaxation techniques and regular, with partner, skills for labour sessions
Tuesdays 18.15-19.45 at the Kindermusik studio, second floor, Leimgrubenweg 9, 4053 Basel
Day time sessions also possible, please get in touch to discuss
25 CHF per session
More details here:
To reserve a place in an upcoming RSB session please use this registration form:
https://forms.gle/MuJJ2XRndYtoDFyw7
Connected and Contented Baby Sessions

Connected and Contented Baby sessions run every Friday 9.30-10.30 at the Magical Café in Felix Kampfplatz.
These sessions combine Baby Yoga, Baby Massage and Baby Signing for a wonderful session that builds connections within the babies' brains, their bodies, with their caregivers and with each others. Suitable for babies and toddlers of all ages.
To reserve a place in a session please use this form:
https://forms.gle/kTDufPNcTsudn1Vr7
Sessions cost 25 CHF per session. Book and pay for multiple sessions of Mother and Baby Yoga and/or Connected and
Contented Baby sessions with a special price:
3 sessions 70CHF
4 sessions 90 CHF
5 sessions 110 CHF
6 sessions 130 CHF
Mama and Baby Yoga

If you have a baby that is already mobile (crawling or walking) and you would like to join a Mama and Baby Yoga series with them please get in touch with me.
Register here: https://forms.gle/hHLHZVwuNKhykW9G8
For more information about prenatal and postnatal classes please see www.mignonbaby.com
Preparing for Parenthood antenatal courses

One to one and small group classes held regularly throughout the year, these classes give your family the support, resources, information and time to understand and plan what you want and need as you become parents.
Sessions typically include topics such as:
Normal process of birth and the Swiss maternity and postnatal care system, including different birth routes, pain management, caesarean birth
Informed decision making and support in developing plans for birth and postnatal period that suits you and your family
Skills and resources for all members of the family to facilitate birth and the postnatal period
Understanding and techniques for successful and well supported breastfeeding, including managing feeding in the family dynamic and when returning to work
Resource, techniques and support for all the family during the fourth trimester and beyond, including use of baby slings
Please contact me directly on antenatal.bct@gmail.com of via the contact form for more details